Dr Aveni Koza
MD, DNB (Dermatology)
Diabetes is one of the commonest medical conditions plaguing the modern era & the incidence is only increasing with time in our society with our sedentary lifestyle & food habits. Like many other long-standing conditions, it often goes undetected for many years until the body starts manifesting with problems that can no longer be ignored- increased thirst, frequent urination, tiredness, weight loss, more hunger, blurred vision and skin problems.
Your skin can give important clues to underlying diabetes (undiagnosed diabetes or pre-diabetes) or indicate uncontrolled sugar levels in confirmed diabetics & the risk of developing complications in which case diabetes treatment needs to be adjusted.
Skin lesions are frequently seen in diabetic patients, from simple skin tags or skin darkening to more problematic skin ulcers & infections- which are often non-healing and hard to treat unless sugar levels are controlled.
High blood glucose impairs the skin’s ability to heal by decreasing blood circulation and damages skin collagen. Tell your doctor if you have frequent skin infections or slow-healing sores as it can be a sign of undiagnosed diabetes
Some of the common skin conditions in people with diabetes are-
DRY ITCHY& CRACKED SKIN
High blood sugar levels pull fluid from cells and make the body lose fluid through increased urination and evaporation through the skin causing dry skin (Xerosis) as well as cracks (fissures). Nerve damage due to diabetes also impairs sweat making skin dry. Use mild soaps for bathing and moisturize regularly when the skin is still moist. Creams and ointments are better than lotions for dry skin.
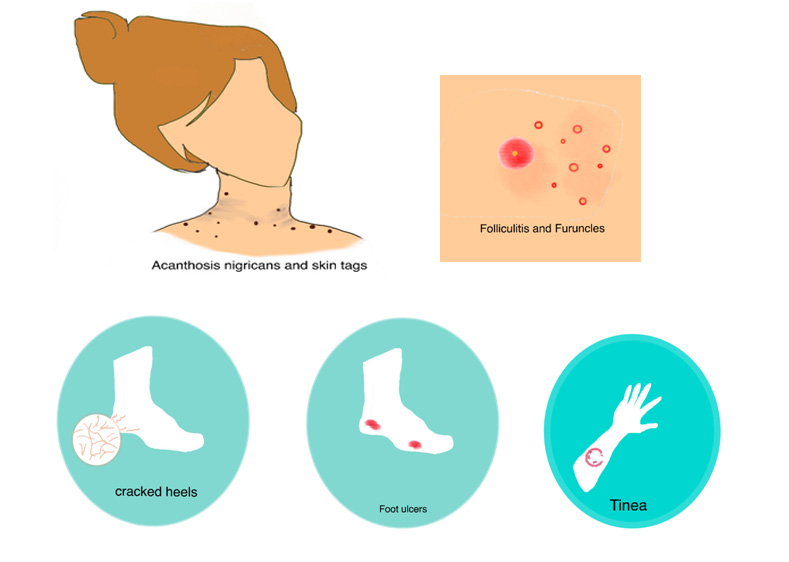
People with diabetes might notice unusualcracked heels due to dryness. Do not attempt to shave or cut away dry skin but gently use a pumice stone right after bathing to remove areas of thickened skin. It is recommended to apply cream containing urea (10-25%) daily.
SKIN TAGS
Skin tags or acrochordons are common noncancerous skin growths seen on the face, eyelids, neck, armpit and groin which are harmless and painless.
It can be tempting and may sound simple to remove it with scissors, nail clippers or blade at home (DIY surgeries!) but can result in deep seated infection, bleeding and unsightly scars.It is best to leave it to a professional dermatologist who will remove the skin tag without causing damage.
SKIN DARKENING & THICKENING
Acanthosis nigricans (AN) is a common condition seen in neck creases, armpits & groin areas which is often mistaken to be due to dirt and scrubbing it hard is only going to make it worse as it is due to dryness & thickened skin. This may be the first sign of diabetes and it is also seen in obesity, polycystic ovarian syndrome and thyroid disease. There is also a possible genetic predisposition (hereditary). Treatment consists of treating the underlying cause.
FUNGAL INFECTIONS
Itchy fungal infections called tinea (‘ringworm’) are commonly seen in people with diabetes especially in moist areas of skin such as skin folds, armpits, under the breasts, between the toes and groin.
Inflammation (redness, irritation and swollen) and infection of glans and foreskin can occur in uncircumcised men with high blood sugar levels. Women can suffer from vaginal yeast infection causing thick white vaginal discharge and severe itching.
It is important to recognize and treat fungal infection with the proper medications prescribed by a dermatologist as many OTC drugs can further aggravate it and complicate its management.
Get immediate medical care if you notice any of the following:
• skin around nail is swollen, red or painful
• filled with pus/crust
• thickened or discolored nail
BACTERIAL INFECTIONS
Increased blood glucose levels allow skin bacteria to grow by decreasing immunity. If you have diabetes, you might often suffer from folliculitis (red bumps with pus around hair) usually after shaving. Infected skin may become swollen, hot, red and painful called furuncles (‘boils’). You’ll need proper antibiotics to get rid of the infection.
Seek immediate medical attention if wounds following a trauma/cut/burn fails to heal or heal slowly.
FOOT ULCERS
The so-called diabetic foot is a persistent ulcer caused by unnoticed injury due to nerve damage (decreased sensation), poor circulation and poor immunity. A deep-seated infection if not treated immediately but allowed to progress to gangrene can lead to amputation of foot.
People with diabetes should check their feet daily for sores, blisters, cuts, corns or redness.
SKIN BLISTERS
Diabetic bullae are skin blisters usually seen on legs, hands, forearms and feet that occur suddenly (without any cause) and resemble burns but without pain or redness. See a dermatologist to correctly diagnose it from other similar skin blistering disorders as treatment differs in other conditions.
PREVENTION & CARE
• Regular medication & controlled diet with a healthy lifestyle.
• Keep skin dry around the moist folds of skin
• Do not try to remove a skin tag
• Treat wounds immediately with proper medications
• Check feet everyday for any cuts or bruises if you have diabetes
Following a basic skin routine can help you prevent skin complications due to diabetes.
Consult your dermatologist to know more about skin management with diabetes.
The writer is Senior Resident, Department of Dermatology, Venereology, Leprology & Cosmetology, CIHSR.