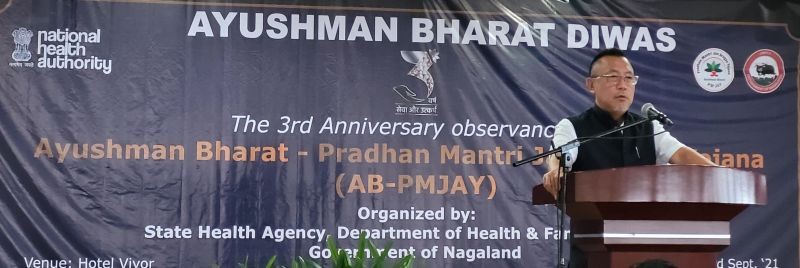
Minister S Pangnyu Phom speaking at the 3rd anniversary observance of AB-PMJAY held at Hotel Vivor, Kohima on September 23. (Morung Photo)
Registered building and other construction workers to join scheme
Our Correspondent
Kohima | September 23
Nagaland Health & Family Welfare Minister, S Pangnyu Phom today said that Ayushman Bharat-Pradhan Mantri Jan Arogya Yojana (AB-PMJAY) scheme has immensely helped beneficiary families from Nagaland who have availed the scheme's benefits either in Nagaland or in other states.
Speaking at the 3rd anniversary observance of AB-PMJAY here at Hotel Vivor, the minister said that Nagaland was among the first states to launch AB-PMJAY in the state on September 23 in 2018.
Stating that AB-PMJAY is the largest public health insurance scheme in the world, he said, in Nagaland it covers 2.33 lakh households, which translates to about 60% of the total population.
He said that Ecard has been issued to 2.6 lakh individuals and reaching 96,000 households which translates to 41% of the target families.
Road ahead
Pangnyu said that building and other construction workers registered under the Department of Labour will soon join the scheme, and accordingly 8584 new families will be added in the state.
Integration with National Food Security Act (NFSA) data is under process whereby the Aadhaar seeded ration cards will be linked to PMJAY portal and thereby ease the enrollment process and improve coverage, the minister said.
The Minister informed that the Nagaland State Rural Livelihood Mission (NSRLM) will be partnering with State Health Agency PMJAY to spread awareness about the scheme through Self Health Groups and also enrollment and Ecard generation through their block data operators.
“Aapke Dwar Ayushman is a new initiative to carry out enrollment drives in the villages to increase Ecard generation. State Health Agent and PMJAY along with various partner agencies will be carrying out these outreach drives till March 2022. It is targeted to reach at least 70% of the total target families,” the minister said.
Appeal for universal health care
Meanwhile, the minister appreciated the State Health Agency led by Principal Secretary Amardeep Singh Bhatia, Department of Health & Family Welfare who is also the CEO of PMJAY, for successful implementation of the scheme in the state.
He thanked the insurance company partners-The Oriental Insurance Company Limited and the Paramount TPA for prompt and tireless support in serving the people of Nagaland, particularly the deprived and vulnerable families which are given health insurance cover through this scheme.
He thanked the Common Service Centers, UTIITSL, Clairvoyance Technologies Pvt Ltd Nagaland, and various partner NGOS for participating in PMJAY ecard generation. “I thank the hospitals implementing this scheme, and particularly the private hospitals which are on board. I appeal to the private hospitals in Nagaland which are yet to join the scheme,” he said.
Stating that there are very few private hospitals in Nagaland, and public hospitals providing secondary and tertiary medical care are also very less, Pangnyu appealed the concerned to consider this as a social responsibility to the people, to come onboard and join the government and implement this scheme “as we strive towards the goal of universal health care.”
Reduce out of pocket expenditure on medical care
Later, Amardeep Singh Bhatia said that Ayushman Bharat is a flagship programme of Ministry of Health & Family Welfare, Government of India. It has two components: Health and Wellness Centres, which is for primary healthcare (and comes under NHM) and PMJAY which is a health insurance scheme for secondary and tertiary care.
He said PMJAY aims to reduce out of pocket expenditure on medical care among poor, deprived and vulnerable families so that they don't experience catastrophic health expenditure and impoverishment.
He said that COVID has severely affected the scheme uptake in 2020 as the district hospitals which take in most of the PMJAY benefits in many districts were converted to COVID hospitals.
He said that a total of 9950 claims amounting to Rs 12 crore were availed during financial year 2019-20. This came down to 7,252 claims amounting to Rs 10 crore in 2020-2021.
“With alternative arrangement to resume non-COVID essential health services, we hope to see improvement in performance,” he said.
Bhatia said that PMJAY scheme shows promising sign as a model of delivering secondary and tertiary healthcare, adding that the current medical reimbursement system for government employees, or other socio-economic categories which are not covered by any medical insurance currently; could all come under the PMJAY platform.
PMJAY is playing a vital role in the road towards achieving universal health coverage, he added.
Earlier, two beneficiaries Khekiye and Y Watimongba shared testimony. The function was chaired by Alongla Aier, technical consultant (PwC) while vote of thanks was proposed by Dr Kika Longkumer, joint director & SNO AB- PMJAY.