Limatula Yaden
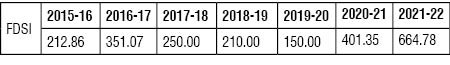
NHM Free Drugs Services Initiative (FDSI)
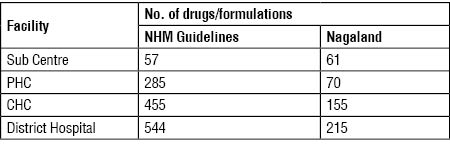
Funding is provided for this Initiative to improve access to and provision of essential drugs/medicines free of cost in all public health facilities to reduce high out of pocket expenditure. There is no prescribed list and free essential drugs/medicines is to be provided to all who visit public health facilities as per State Essential Drug List. The indicative numbers as per NHM Guidelines and Nagaland are:
Guidelines are available at:
http://nhm.gov.in/nhm_components/Health_Systems_Strengthening/Drugs_&_Logistics/Operational_Guidelines_Free_Drugs_Service_Initiative.pdf
Approvals given for Free Drug Service Initiative to Nagaland are as follows:
(Rs in lakhs)
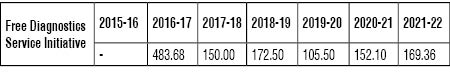
Free Diagnostic Services Initiative
The objective is to reduce out-of-pocket expenditure on diagnostics as well as improve quality of care by providing accurate diagnosis. Funding is given to provide free essential diagnostics in public health facilities. There is no prescribed list of essential diagnostics. Facility wise indicative number of essential diagnostics as per guidelines is as below:
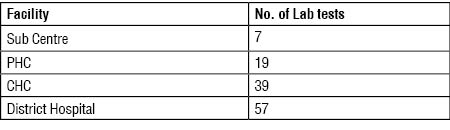
While approval has been given, the State is yet to fully implement this initiative. The guidelines are at:
http://nhm.gov.in/nhm_components/Health_Systems_Strengthening/Diagnostics/Free_Diagnostics_Service_Initiative.pdf
Approvals given for Free Diagnostics Service Initiative to Nagaland are as follows:
(Rs in lakhs)
Pradhan Mantri National Dialysis Programme (PMNDP)
Under this Programme’, funding is provided to States for provision of free dialysis services to the poor. Approvals given to Nagaland are as follows:
(Rs in lakhs)
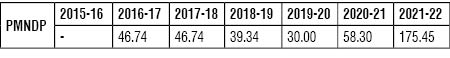
Nagaland is also one of the 10 States selected for 14(9+5) free dialysis machines donated by M/s Fairfax India Charitable Foundation. This was facilitated by NHM to enable State to provide free dialysis services to the poor.
National Ambulance Services
One of the most visible components of NHM is the free patient transport ambulances operating under Dial 108/102. Dial 108 is emergency response system, primarily designed to attend to patients of critical care, trauma and accident victims etc. Dial 102 services are essentially aimed at catering to needs of pregnant women, children though other categories are not excluded. Funding is given for both Basic Life Support(BLS) and Advance Life Support (ALS) vehicles.BLS unit should have two Emergency medical Technicians while ALS unit should have a paramedic apart from the Emergency medical Technician apart from being equipped with airway equipment, cardiac life support, cardiac monitors and glucose testing device.
Approvals given to Nagaland in last seven years are as follows:
(Rs in lakhs)
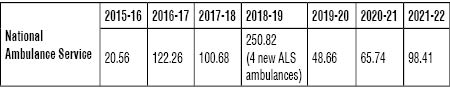
Nagaland has reported 82 operational ambulances as on September, 2019.
http://164.100.24.220/loksabhaquestions/annex/173/AU2636.pdf
National Mobile Medical Unit Services (MMU)
Funds are given for MMUs with the objective of taking healthcare to the doorstep of the public and to provide a whole range of health care services –free treatment of minor ailments, communicable & non communicable diseases, Reproductive & Child Health, Family Planning and diagnostics services. States/UTs have been given flexibility to deploy Mobile Medical Units (MMUs) to provide a range of health care services for the populations particularly living in remote, inaccessible, un-served and underserved areas, as per the needs identified by the respective States.
Deployment of MMUs is 1 MMU/ 10 lakh population subject to a cap of 5 MMUs/district. Additional MMU can be supported where one MMU exceeds 60 patients/ day in plain areas and 30 patients/day in hilly areas. Support includes both capital cost and operational cost (Human resource, drugs, consumables etc).Approvals given to Nagaland are as follows:
(Rs in lakhs)
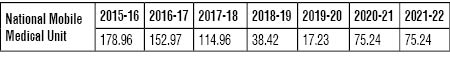
Nagaland has reported 7 operational MMUs as on September, 2019 http://164.100.24.220/loksabhaquestions/annex/173/AU2636.pdf
Janani Suraksha Yojana (JSY)
JSY is a safe motherhood programme to reduce maternal and neonatal mortality by promoting delivery in public health facilities. ASHAs and pregnant women are provided Cash Assistance for Institutional Delivery and post delivery care as under:
In Rupees
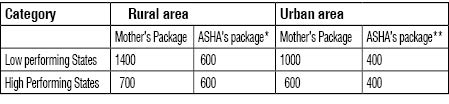
* ASHA package in rural areas include Rs. 300 for ANC component + Rs. 300 for facilitating institutional delivery.
** ASHA package of Rs. 400 in urban areas include Rs. 200 for ANC component + Rs. 200 for facilitating institutional delivery.
Approvals given to Nagaland are as under:
(Rs in lakhs)
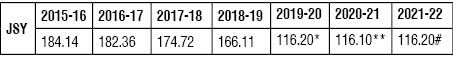
*does not include Rs 42 Lakh approved for ASHA incentive to facilitate institutional deliveries in Govt. Health facilities.**does not include Rs 38.40 Lakh approved for ASHA incentive to facilitate institutional deliveries in Govt. Health facilities.#**does not include Rs 38.40 Lakh approved for ASHA incentive to facilitate institutional deliveries in Govt. Health facilities.
Janani Shishu Suraksha Karyakram (JSSK)
This scheme entitles all pregnant women delivering in public health facilities to absolutely free and no expense delivery including Caesarean section for which funds are provided under NHM :
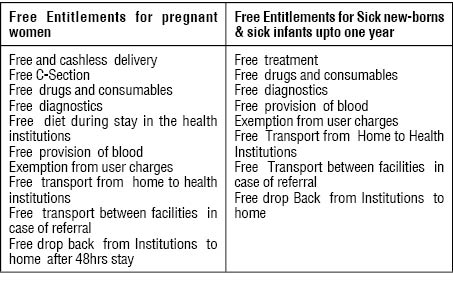
Approvals given to Nagaland in the last seven years are as below:
(Rs in lakhs)
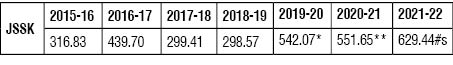
* includes Rs 286.00 lakh for Free drugs and consumables under JSSK, Rs 70 Lakh for Free diagnostics for Pregnant women under JSSK, Rs 2.5 Lakh for Free Diagnostics for Sick infants under JSSK, Rs 170 Lakh for Free Referral Transport – JSSK for Pregnant women, Rs 25 Lakh for Free referral Transport – JSSK Sick infants, Rs 57.60 Lakh for Diet services for JSSK beneficiaries, 0.97 Lakh for Blood transfusion for JSSK beneficiaries.
** includes Rs 246.65 lakh for Free drugs and consumables under JSSK, Rs 59 Lakh for Free diagnostics for Pregnant women under JSSK, Rs 2.5 Lakh for Free Diagnostics for Sick infants under JSSK, Rs 160 Lakh for Free Referral Transport – JSSK for Pregnant women, Rs 25 Lakh for Free referral Transport – JSSK Sick infants, Rs 57.60 Lakh for Diet services for JSSK beneficiaries, 0.90 Lakh for Blood transfusion for JSSK beneficiaries.
# includes Rs 255.14 lakh for Free drugs and consumables under JSSK, Rs 58 Lakh for Free diagnostics for Pregnant women under JSSK, Rs 2.5 Lakh for Free Diagnostics for Sick infants under JSSK, Rs 196 Lakh for Free Referral Transport – JSSK for Pregnant women, Rs 35 Lakh for Free referral Transport – JSSK Sick infants, Rs 81.90 Lakh for Diet services for JSSK beneficiaries, 0.90 Lakh for Blood transfusion for JSSK beneficiaries.
RASHTRIYA BAL SWASTHYA KARYAKRAM (RBSK)
Funds under RBSK are provided for free Screening and early Intervention of children for early detection and management of 4 Ds i.e. Defects at birth, Diseases, Deficiencies, Development delays including disability and free treatment of 30 identified health conditions including free surgery at tertiary health facilities(e.g. conditions like congenital heart disease, cleft lip and correction of club foot etc. The details are available at:
http://nhm.gov.in/images/pdf/programmes/RBSK/For_more_information.pdf
National Vector-Borne Disease Control Programme
This is an umbrella programme with an integrated approach for elimination of Malaria, Lymphatic Filariasis, Kala-azar and control of Dengue, Chikungunya and Japanese Encephalitis)
Malaria
Following services are provided free by Government:
i) Prevention of mosquitogenic conditions by source reduction activities, Larvivorous fish, anti larvals, Indoor Residual Spray (IRS) and distribution of Long Lasting Insecticidal Nets (LLIN) in high risk population
ii) Early detection of malaria cases by Microscopy or Bivalent Rapid Diagnostic Tests (RDT)
iii) Complete treatment of malaria cases-both Plasmodium vivax and Plasmodium falciparum cases
National Tuberculosis Elimination Programme (NTEP)
Funds are provided for free diagnosis and treatment of Tuberculosis including Drug Resistant TB including high quality drugs free of cost through community providers closest to the residence of the patient.
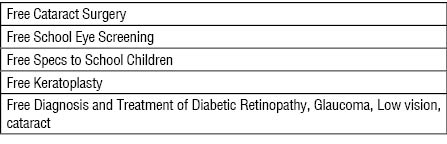
National Programme for Control of Blindness
Funds are provided for the following:
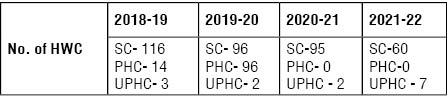
Ayushman Bharat -Health and Wellness Centres (HWC)
Government launched Ayushman Bharat in 2018-19 with two components, namely, the Pradhan Mantri Jan Arogya Yojana and Health and Wellness Centres to provide comprehensive primary care services.
Existing Sub Centre and PHC/ Urban PHC are to be strengthened as HWCs. Sub centre level HWC should have a Mid-level healthcare Provider, who can be BSc in Community Health/Ayurveda practitioner or Nurse trained in a six-month certificate course in Community Health through IGNOU. HWCs are to provide Preventive, promotive, rehabilitative and curative care for RMNCH+A, Communicable diseases, non-communicable diseases, Ophthalmology, ENT, Dental, Mental, Geriatric care, Palliative care, treatment for acute simple medical conditions and basic emergency & trauma services.
To begin with, HWCs have to initiate free Universal Screening and treatment including monthly refill of drugs for five common Non Communicable Diseases - Hypertension, Diabetes, and Cancer of the Breast, Cervix & Oral. i.e. all population (men and women) above 30 years are to be screened and treated free of cost for these common NCDs.
The PHCs upgraded as HWC should provide services as per IPHS.
Approvals given to Nagaland are as follows:
Community Process and Social Accountability
At the time of launch of the National Rural Health Mission (NRHM), which later got subsumed as one of the two submission of the overarching National Health Mission (NHM), community ownership of the health delivery system was envisaged as one of the pillars on which the super-structure of the NRHM would be built. The community should emerge as active subjects rather than passive objects in the context of the public health system" - NRHM Framework for Implementation, MoHFW, GoI, 2005-2012. Thus NHM places strong focus on community engagement for people’s participation in health and social determinants of health as well as improve governance through community ownership and participation. The ASHA, the Village Health Sanitation and Nutrition Committee (VHSNC), public participation in facility based committees are aimed at community mobilization for health and other social determinants of health.
1. ASHAs
Roles and responsibilities of an ASHA include that of a healthcare facilitator, a service provider and a voluntary health activist. She is expected to fulfill her role through five tasks:
(i) Home Visits: For two to three hours every day, for at least four or five days a week, ASHAs should visit families living in her allotted area. Where there is a newborn in the house, six visits or more becomes essential.
(ii) Village Health and Nutrition Day (VHND): To attend &promote attendance at the monthly VHNDs
(iii) Visits to health facility: This usually involves accompanying pregnant woman, sick child, or some member of the community needing facility based care besides attending monthly PHC review meeting.
(iv) Holding village level meeting: As a member of the Village Health, Sanitation and Nutrition Committee, she is expected to call its monthly meeting.
(v) Records: Maintain records to make her more organised
ASHA is to provide community level care for minor ailments such as diarrhoea, fevers, care for the normal and sick newborn, childhood illnesses and first aid. She is also a provider of DOTS under RNTCP, doorstep delivery of contraceptive services (OCP, Condoms and EC). She is to inform about births and deaths in her village and any unusual health problems/disease outbreaks in the community to the Sub Centres/PHC.
The ASHA is also intended to facilitate access to health services, mobilize communities to realize health rights and access entitlements and provide basic community level care, the other elements focus on promoting action by village level organisations and enhance people’s participation in service delivery. (http://nhsrcindia.org/community-processes)
VILLAGE HEALTH SANITATION AND NUTRITION COMMITTEES (VHSNC)
VHSNC is a key communitisation Platform for Collective Community Action, on issues related to health and its social determinants. The VHSNC should have a minimum of about 15 members and its composition are as under:
• Elected Gram Panchayat members
• ASHAs (Member-Secretary and Convenor of VHSNC)
• ANM, AWW, School teacher provided they are resident in the village. Otherwise they qualify as special invitees.
• Community based organizations
• Service users
VHSNCs are provided with an annual untied grant of Rs 10000 to be credited to bank account andoperated by Chairperson, VHSNC and Member Secretary as joint signatories. Untied grants is topped up based on utilization.VHSNCs can undertake activities like cleanliness drives, sanitation drives, chlorination of water, repair of water facilities and drainage system, Information, Education and Communication activities. VHSNCs are required to inform about their activities and expenditures and regarding creation of facilities, infrastructure, available benefits and names of beneficiaries under the scheme to the villagers in their bi-annual meetings and the Gram Panchayat in their quarterly meetings besides monitoring public services viz, health services, MNREGA, Mid day meals, PDS, access to drinking water, toilets etc Guidelines are available are
http://nhm.gov.in/images/pdf/communitisation/vhsnc/Resources/Handbook_for_Members_of_VHSNC-English.pdf
Nagaland has reported that 1346 VHSNCs have been constituted as on September,2019.
(http://164.100.24.220/loksabhaquestions/annex/173/AU2636.pdf)
Rogi Kalyan Samiti (RKS)
RKS/Patient welfare Committees are to be constituted at level of PHC and above. They are required to be registered under Societies Registration Act and with account in a local bank. RKS consists of members from local Panchayati Raj Institutions, local MP/District Magistrate, NGOs, local elected representatives and state Government officials. The RKS sare to act as a forum to improve the functioning and service provision in public health facilities, increase participation and enhance accountability for provision of better facilities to the patients. . As laid out in the RKS guidelines issued in 2015, the RKS is to play a supportive and complementary role to the hospital administration in ensuring the provision of universal, equitable and high quality services, and in ensuring support services in addition to holding the administration accountable keeping the centrality of patient welfare in mind.Untied grants to public health facilities are to be administered by RKS.
Guidelines are at https://nhm.gov.in/images/pdf/NHM/NHM-Guidelines/Rogi_Kalyan_Samities.pdf Nagaland has reported that 167 Rogi Kalayan Samities have been constituted. http://164.100.24.220/loksabhaquestions/annex/173/AU2636.pdf
(The writer is Additional Director General, DGHRD, Central Board of Indirect Taxes and Customs and served as Director NHM Policy, Ministry of Health and Family Welfare, Government of India for over 6 years . The views expressed are personal)