Limatula Yaden
Public Health is a state subject and hence the primary responsibility to provide accessible, affordable quality heathcare to the population lies with the State Government. Under the National Health Mission (NHM), the Central Government supplements the efforts of the state by providing support (Both financial and technical ) under the Mission.
The information on approvals given to States/UTs including Nagaland under NHM are available at
https://nhm.gov.in/index4.php?lang=1&level=0&linkid=66&lid=79
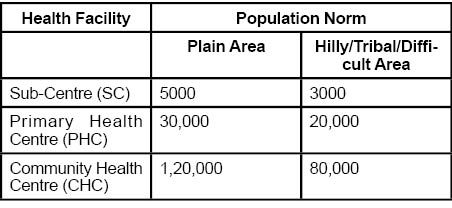
Indian healthcare infrastructure in rural areas is designed as a three tier system on a population norm as follows:
Sub Centre
Sub Centre is first point of contact between primary healthcare system and community. Due to scattered /wide dispersal of population and hilly/difficult terrain, a new norm ‘ Time to care’ was adopted for establishing Sub Centre for hilly and Desert areas. Accordingly irrespective of population size, a Sub Centre can be established within 30 minutes by walk from habitation.
Sub centres are to be staffed by at least one Multi-Purpose Worker (Female) commonly known as ANM and one Male Health worker. Sub centres are provided with basic drugs for minor ailments to take care of essential health needs of population. The Indian Public Health Standards (IPHS) 2012 categorizes Sub Centres into 2 Types. The difference between Type A and Type B Sub-centres, is that the latter is envisaged to have facilities for conducting deliveries. Wherever two ANMs are provided, one ANMs is required to be available at Sub-centre which is to remain open for OPD services on all working days while second ANM provides outreach services. ANMs posted at Type B centres must be trained in Skilled Birth Attendance.
Key Essential services to be provided by SC as per IPHS include:
• Maternal Health services: Early registration of pregnancies, within first trimester before 12th week of Pregnancy, Minimum 4 Ante Natal Checks including Registration, general examination such as height, weight, B.P., anaemia, abdominal examination, breast examination, Folic Acid Supplementation (in first trimester), Iron & Folic Acid Supplementation from 12 weeks, injection tetanus toxoid, treatment of anaemia etc, post-natal home visits on 0,3,7 and 42nd day
• Child Health services: Newborn Care -maintain the airway and breathing, initiate breast feeding within one hour, infection protection, cord care, care of the eyes, full Immunization;
• Family Planning Services: Provision of contraceptives such as condoms, oral pills, emergency contraceptives, Intra Uterine Contraceptive Devices (IUCD) insertions wherever ANM is trained in IUCD insertion.
• Curative Services: Treatment for minor ailments including fever, diarrhea, ARI, first Aid and prompt referral
• Home Visits: Post-natal and newborn visits – as per protocol, check out on disease incidences, notify M.O. PHC immediately about any abnormal increase in cases of diarrhoea/dysentery, fever with rigors, fever with rash, etc
Primary Health Centre
The PHC with 6 indoor beds is first contact point between community and Medical Officer. A PHC should have one MBBS doctor, three Staff Nurses, One pharmacist and a Lab Technician among others. It acts as referral unit for 6 Sub-Centres and refer out cases to CHC and higher level facilities. Essential medical care services required to be provided by a PHCs as per IPHS include:
• OPD services: Total 6 hours of OPD services - 4 hours in morning and 2 hours in afternoon for six days/week as per time schedule set by state. Minimum OPD attendance expected is 40 patients per doctor/day.
• 24 hours emergency services: appropriate management of injuries and accident, First Aid, stitching of wounds, incision and drainage of abscess, stabilisation of patient before referral, Dog bite/snake bite/scorpion bite cases, and other emergency conditions to be provided primarily by the nursing staff. However, MO may be available to attend to emergencies on call basis.
• Referral services.
• In-patient.
Nagaland has reported 33 PHCs working on 24x7 basis.
http://164.100.24.220/loksabhaquestions/annex/173/AU2636.pdf)
Community Health Centre
CHCs constitute first secondary level healthcare, and provides referral as well as specialist services. A CHC is a 30 bedded facility with one OT, X-ray, Labour Room and Laboratory facilities and is required to be staffed by four Medical Specialists i.e. Surgeon, Physician, Gynecologist and Pediatrician supported by paramedical and other staff. It serves as a referral centre for 4 PHCs and also provides facilities for obstetric care and specialist consultations. Essential services includes routine and emergency care in Surgery, Medicine, Obstetrics and Gynaecology, Paediatrics, Dental and AYUSH .
Detailed information are at http://www.nhm.gov.in/images/pdf/guidelines/iphs/iphs-revised-guidlines-2012.
Untied Grant (UG) to Facilities
One of the critical components of NHM is provision of Untied Funds to public health facilities for local planning and action. This is to provide flexibility from rigid line item budgeting and can be used for minor repair and maintenance work, purchase/maintenance of light bulbs, inverter, office stationaries, purchase and repair of minor medical equipment, patients welfare etc.
The quantum of untied grants provided to facilities are as below:
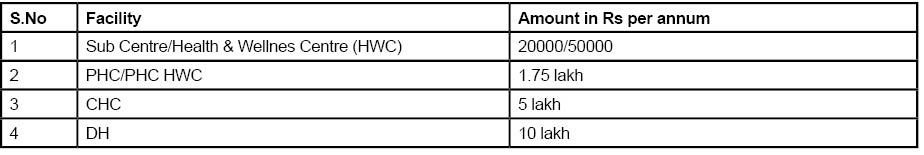
Untied grants are provided on the principle of ‘ Top up’ based on fund utilization.
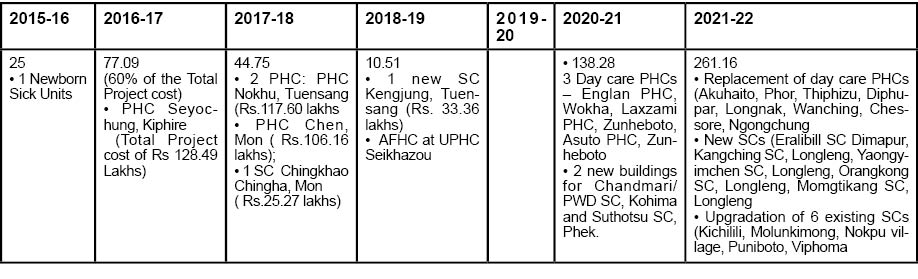
Infrastructure approvals in the last seven years are as follows:
(Rs in lakhs)
Major Upgradation
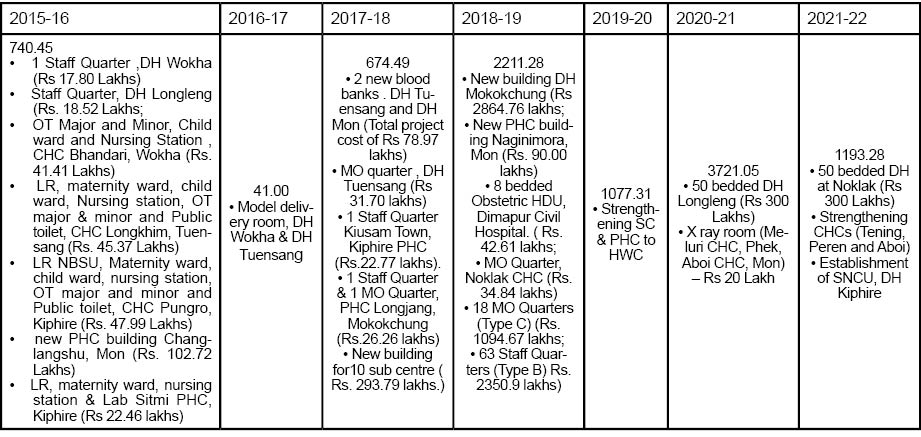
New Construction
(Rs in lakhs)
State Plans (PIPs) & approvals (RoPs) are available at http://nhm.gov.in/nrhm-in-state/state-program-implementation-plans-pips.html
FORWARD LINKAGES TO NRHM SCHEME
NHM funds only primary & secondary care upto District Hospital (DH) level. As a special dispensation for NE states, 100% funding was provided for strengthening Tertiary / Secondary level health infrastructure. Six projects approved are:
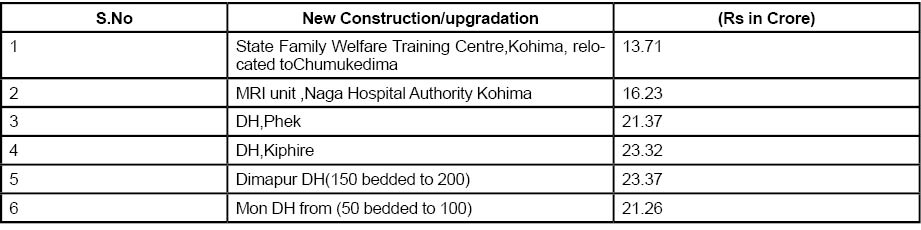
The Scheme has been approved by the Government for implementation upto 2018-19 for Ongoing projects only.
(The writer is Additional Director General, DGHRD, Central Board of Indirect Taxes and Customs and served as Director NHM Policy, Ministry of Health and Family Welfare, Government of India for over 6 years . The views expressed are personal)